Roux-En-Y Gastric Bypass
What is the Roux-En-Y Gastric Bypass?
The ROUX-EN-Y GASTRIC BYPASS, also known as the GASTRIC BYPASS procedure has been performed for approximately 4 decades throughout the world. It is the oldest weight loss operation that is still performed.
During the ROUX-EN-Y GASTRIC BYPASS a small stomach pouch (residual stomach capacity of 30-50mls) is created to restrict food intake. Next, a Y-shaped section of the small intestine is attached to the pouch to allow food to bypass the lower stomach, the duodenum (the first segment of the small intestine), and the first portion of the jejunum (the second segment of the small intestine).
Food and nutrients therefore do not pass through the first 150-200cm of the intestine. This bypass reduces the absorption of food and nutrients from the first 150-200cm of the intestine, thereby reducing the calorie intake.
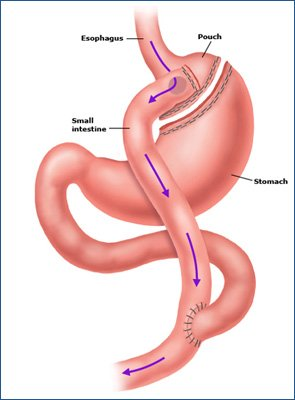
Ultimately food reaches to distal part of the small intestine faster, thereby causing the release of certain hormones from the cells in this part of the intestine, which then act to feedback to the brain and stomach causing reduced hunger and emptying of the stomach.
The Roux-en-Y Gastric Bypass, because of its ability to reduce absorption of nutrients in the intestine, is considered a more powerful weight loss procedure than a Gastric Sleeve, often leading to greater weight loss than a Gastric Sleeve.
The Roux-en-Y Gastric Bypass is a less restrictive procedure than a Gastric Sleeve but in a different way to the Gastric Sleeve procedure.
It is also preferred by many surgeons as the revisional procedure of choice for patients who have a failed Gastric Band, or complications following Sleeve Gastrectomy such as severe gastro-oesophageal reflux or weight regain.
What are the Advantages of the Gastric Bypass?
| Lose more weight than GASTRIC BAND OR GASTRIC SLEEVE |
|---|
| Long track record with proven long term weight loss |
| Preferred Bariatric procedure for patients with TYPE 2 DIABETES |
| Remission of TYPE 2 DIABETES - better than GASTRIC SLEEVE |
| Preferred Bariatric procedure for patients with SEVERE GASTRO-OESOPHAGEAL REFLUX |
| Preferred Bariatric procedure for patients with BARRETT’S OESOPHAGITIS |
| Preferred Bariatric procedure for patients with SUPER OBESITY BMI >50 |
| Effective for those with high sugar or high fat diet. Dumping syndrome is directly linked to a high sugar or high fat intake. Symptoms of dumping are unpleasant and therefore discourage the intake of high calorie sweet foods. |
| Revision surgery for failed GASTRIC BAND or GASTRIC SLEEVE or for those suffering from severe reflux or weight-regain |
How Much Weight Will I Lose with the Gastric Bypass?
The Laparoscopic Gastric Bypass operation is arguably the gold standard weight loss operation with an estimated weight loss of 70-80% EWL (excess weight loss) over 2 years.
Who is a Candidate for Roux-En-Y Gastric Bypass?
The Roux-En-Y Gastric Bypass may be performed on any patient who is eligible for weight loss surgery.
It is often performed in Australia as a primary weight loss procedure in patients with Type 2 Diabetes. Current published randomized controlled trials have shown that obese patients who have had Type 2 Diabetes for many years and are on insulin or many different diabetic medications are more likely to have their diabetes go into remission, stay in remission, and require fewer medications for their diabetes than patients having the Sleeve Gastrectomy.
It is also performed on patients who have severe gastro-oesophageal reflux, as the stomach acid empties more rapidly out of the stomach into the intestine with a Roux-en-Y Gastric Bypass and is therefore less likely to reflux back up into the lower oesophagus and cause reflux symptoms.
It is also preferred in patients with higher BMI’s or those that typically need to lose more than 50kg of excess weight, as this may be more difficult to achieve with a Gastric Sleeve procedure.
It is also commonly performed as a revisional or second procedure on patients who have been unsuccessful with GASTRIC BANDING or SLEEVE GASTRECTOMY or patients who have developed severe Gastro-oesophageal reflux after Gastric Sleeve surgery.
The Roux-En-Y Gastric Bypass is not advisable for patients who are smokers or have Crohn’s disease, and may not be possible in any patient with extensive previous abdominal surgery.
What are the Disadvantages of the Gastric Bypass?
| Not recommended in smokers due to the risk of Stomal Ulcer formation at the join between the stomach and intestine |
|---|
| Not recommended in patients with Crohn's disease. |
| Not recommended in patients taking Immunosuppression medication, eg following Liver or Kidney Transplant. |
| The ROUX-EN-Y GASTRIC BYPASS is a more complicated procedure and is technically more difficult to perform than GASTRIC BAND and GASTRIC SLEEVE |
| It has a higher risk of EARLY COMPLICATIONS - staple line bleed or leak, anastamotic strictures, long anaesthetic, higher risk of blood clots in legs or lungs |
| It has a higher risk of LONG TERM COMPLICATIONS than GASTRIC BAND and GASTRIC SLEEVE including stomal ulcers, dumping syndrome, internal hernias, and vitamin and nutritional deficiencies, anastamotic dilatation. |
| Nutritional & mineral supplements required INDEFINITELY in all patients following surgery. |
| DUMPING SYNDROME is common after GASTRIC BYPASS and occurs in patients if they consume any rich or sweet liquids or sweet solid food. This may be beneficial for patients as it deters them from consuming these types of liquids or foods. It is an unpleasant sensation of sweating, shakiness, light headedness, weakness, palpitations, abdominal cramps, and diarrhea, and occurs minutes to hours after eating. Sometimes these symptoms are so severe that they may cause convulsions or fainting. |
| The GASTRIC BYPASS may rarely need to be reversed in severe cases of Dumping syndrome or recalcitrant stomal ulcers. |
What are the Risks of a Roux-En-Y Gastric Bypass?
As with any surgical procedure, the GASTRIC BYPASS operation has risks which are important to clearly understand before proceeding.
The following is a comprehensive list of issues which can occur. Most of these complications are very rare and 90-95% of patients have no issues.
Dr Hatzifotis takes measures directly aimed at reducing these risks, but if complications occur, additional treatment may be necessary.
Possible Acute Complications may include (but are not limited to):
- Bleeding - This occurs in less than 1 in 100 patients after the procedure. This may require blood transfusion or rarely re-operation.
- Leak - A leak of fluid can occur through the new join between the stomach and intestines if it does not heal well. This can happen in the first few days after surgery and may require reoperation. If these leaks persist they can leak to the skin or wound (known as a fistula) or cause a persistent fluid infection in the area (abscess). If this happens, length of hospital stay may be extended to weeks or even months after surgery, and it may be a life-threatening problem. This occurs in less than 1% of cases.
- Other Uncommon Complications - Precautions are taken in all patients to reduce any risks to the absolute minimum. The following complications are uncommon & unusual, and may occur following any surgical procedure:
- Internal injuries to nearby organs such as the spleen
- Bleeding - 1 in 1000 patients
- Blood clots in leg veins, lungs or abdomen - 1 in 1000 patients
- Infections in abdomen, chest or wounds
- Allergic reactions to anaesthesia or medications
Are there any Long term Complications of the Gastric Bypass?
There are some long term problems following the GASTRIC BYPASS that have been reported to date.
Possible long term complications may include (but are not limited to):
- Ulcers - Just like ulcers can occur in a normal stomach, they can also occur in the new stomach pouch after a gastric bypass. For this reason, patients need to take anti-ulcer medication for 3 months after surgery, or even lifelong in some patients. Sometimes ulcers can still develop and require additional therapy to manage.
- Anastomotic Stricture – It is important to keep the new connection between the stomach and the intestines small so as to achieve the right amount of weight loss. Sometimes this means the connection is too tight (1% patients). If this occurs it may require stretching under endoscopy (camera into the stomach) or re-operation
- Internal Hernia – Occasionally the loops of bowel in the abdomen can become entangled and get stuck. If this occurs, a re-operation is required to fix the problem. If there are any unexpected abdominal complaints it is important to be assessed quickly by the surgeon.
- Weight re-gain or Failure of weight loss – This usually occurs when dietary advice is not followed. If you eat too much food at once, this can stretch the small stomach pouch making it easier to take larger volumes at meal times in the future.
- Dumping Syndrome
- Dumping is a group of signs and symptoms that usually occurs due to poor food choices. It is the result of high sugar or high-fat foods passing too quickly into the small intestine. Symptoms can include cramping, nausea, dizziness, weakness and fatigue. More information about dietary advice to avoid dumping will be provided during your visit to the dietitian.

